- Continue Shopping
- Your Cart is Empty
What is Celiac Disease?
Overview of Celiac Disease

Celiac disease has gotten a lot of attention over the past couple of years, but like all things that are a little hard to pronounce, there’s quite a bit of misinformation out there.
You may have heard questions like, “Can people with celiac disease eat quinoa?” and “You’re paleo, you don’t eat gluten; are you celiac?” and “Does that mean you burst into flames upon exposure to cinnamon rolls?” This is all understandable; it’s a fairly complex topic.
In short, celiac disease is an immune reaction in the small intestine to the gluten proteins found in wheat, rye, and barley. Over time, the inflammatory response damages the small intestine and can lead to problems with absorbing nutrients. The gut freaks out and treats gluten as though it’s a vengeful demon and starts attacking both the gluten particles and itself in attempt to perform the exorcism.
Symptoms
When your body freaks out upon ingesting gluten, it can result in a number of less-than-fun symptoms. A classic telltale sign of celiac disease is diarrhea and weight loss caused by the damage to the small intestine.
This “malabsorption” weight loss is not the sexy kind of weight loss. It’s more like the weight loss where you ask, “Where did all my muscle mass go and why did that light breeze knock me over?”
Here’s a laundry list of additional symptoms associated with celiac disease.
- Anemia, usually resulting from iron deficiency
- Loss of bone density (osteoporosis) or softening of bone (osteomalacia)
- Itchy, blistery skin rash (dermatitis herpetiformis)
- Damage to dental enamel
- Headaches and fatigue
- Nervous system injury, including numbness and tingling in the feet and hands, and possible problems with balance
- Joint pain
- Reduced functioning of the spleen (hyposplenism)
- Acid reflux and heartburn
A good percentage of celiac sufferers also report constipation, and are overweight or obese. In children, failure to thrive due to diarrhea is a main symptom.
Another common correlate condition is a blistering, itchy rash that stems from a change in the lining of the small intestine. Whichever symptoms manifest, though, they aren’t very fun.

The Gut Reaction
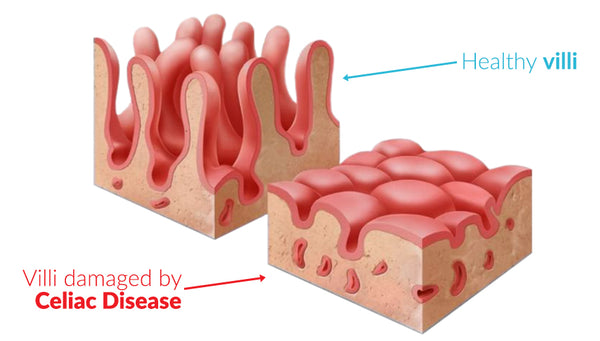
So what actually happens in the gut that causes all of this nonsense? We know that gluten is super damaging in general, but celiac disease takes it to a whole new level. In celiac patients, the autoimmune reaction to gluten damages the lining of the small intestine.
Lining the small intestine are small, finger-like projections called villi that increase the surface area of the gut; imagine a shag carpet lining the gut, with each piece of shag as a nutrient absorbing machine, those are the villi and they do a phenomenal job of transferring nutrients from the food you eat into your body.
Now imagine all those pieces of shag as inflamed and you’ve got the beginning of what celiac disease is like. It gets worse though; the gluten particles first cause inflammation, the inflammation attacks the villi, and the villi, no longer able to absorb nutrients, begin to atrophy and dissolve.
As more and more villi wither away under the onslaught of gluten, there is less and less surface area for nutrient absorption and eventually the gut lining becomes scarred. This leads to malabsorption, then malnutrition, and opens up the possibilities for all those other gnarly symptoms down the line.
Not All Gluten Aversions Are Created Equal
Just because someone avoids gluten does not mean they have celiac disease. Though other digestive issues can be traced to gluten intolerance, celiac disease is a specific type of gluten intolerance characterized by the damage caused to the small intestine.
Some theorize, however, that gluten intolerance is caused by the immune system targeting the actual gluten particles, whereas celiac disease is when the immune system erroneously attacks the small intestine.
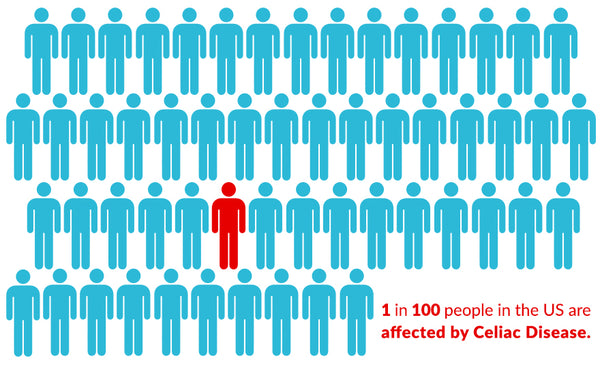
Estimates for the prevalence of celiac disease put it at about 1 in 100 people, but similar guesses as to the exact amount of gluten intolerance in the population are much greater. Some say about 1 in 5 people have some gluten sensitivity, but others say the number is staggeringly higher, as much as 1 in 2.
So all celiac disease is a kind of gluten intolerance, but not all gluten intolerance is celiac disease. Like how all squares are rectangles, but the reverse is not true.
Screening And An Increase in Celiac Disease Frequency
Screening for celiac disease is a little frustrating. The process itself isn’t so bad, but because most of the symptoms associated with celiac are so common, and indicative of other maladies, celiac is often misdiagnosed, or missed completely. This can leave people feeling crappy for extended periods of time with no idea why.
Still, diagnoses of celiac disease are on the rise, with celiac being four times more common than it was 60 years ago.
This could be a result of finding what you’re looking for vs actual cases being on the rise, but gluten is tough for the body to deal with even if it doesn’t cause an autoimmune reaction. Increased screening for celiac disease and gluten intolerance is revealing increased incidents of celiac disease and gluten intolerance, and an estimated 1 in 100 people in the US are celiac.
In Italy, where gluten is a major part of the diet, Celiac (or coeliac) is considered one of the most common chronic disorders.
If you child has any of the above symptoms, it’s fast and easy to find out if they’re just gluten intolerant or have celiac disease.
There is Good News, Though
The good news is that celiac disease is extremely manageable. For the acute inflammation in the gut, a doctor may prescribe steroids to carpet-bomb the autoimmunity out of you.
Short-term catabolic steroids are borderline magical for calming the body down, but the long term solution is even more magical.
The real magic comes from…wait for it…a gluten-free diet.
Remove the source of your gastric distress, the gut heals, and all is well in the small intestine shag carpet kingdom. Italy’s restaurants and grocery stores are excellent about providing gluten-free options for its many celiac sufferers.
Some docs recommend you stay on gluten if you’re going to get yourself tested for celiac disease as being gluten-free can come up with a false-negative. Others say that if you’re already gluten-free, it may not be worth the damage you cause yourself by re-introducing it just to get a test.
And More Good News
Possibly the best news, however, is that you don’t need gluten. Like, at all.
There’s no dietary requirement for it. It’s not nutritious, and it (and the foods that use it) doesn’t contain anything that we as humans can’t get from other sources. Most people feel better when they go gluten-free, even if they don’t have celiac disease or a gluten-intolerance.
Foods that contain gluten are also usually high in carbohydrate and simple sugars, which displace a lot of good foods like healthy meats and vegetables. Centering a diet around nutrient dense foods described in our Paleo Pillars will undoubtedly be healthier than one built on a foundation of gluten and grains.
Hopefully this gives you a better idea of what celiac disease is and is not. It’s not the same as gluten sensitivity, and it’s not the same as Paleo, and it is not the end of the world. There is hope for celiac sufferers and for those who still enjoy a little bit of deliciousness every once in a while.Leslie Blood
Paleo mama Leslie B is a regular contributor to the Paleo Treats blog. She is a recipe wizard and has two full time testers ready to taste everything she makes. Leslie lives in Colorado and in between raising her testers (aka little boys) and work manages to find time to run in the mountains and write down her best recipes.